




Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
An overview of the nursing process, which is a systematic, rational method of planning and providing individualized nursing care. It explains the purpose, phases, characteristics, benefits, and methods of the nursing process. The document also discusses the four types of assessment, data collection, validation, and evaluation. It concludes with a discussion of documentation and reporting, including the purpose and components of client records and documentation systems.
Typology: Lecture notes
1 / 6

This page cannot be seen from the preview
Don't miss anything!



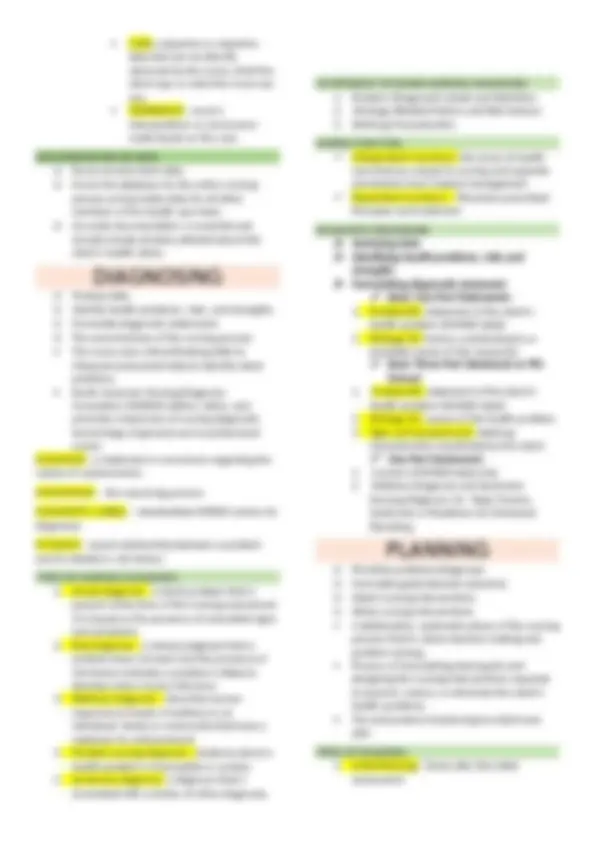
A systematic, rational method of planning and providing individualized nursing care. An organized sequence of problem-solving steps used to identify and to manage the health problems of clients. PURPOSE OF NURSING PROCESS To identify a client’s health status and actual or potential health problems or needs. To establish plans to meet the identified needs. To deliver specific nursing interventions to meet those needs. PHASE OF THE NURSING PROCESS PHASE DESCRIPTION ASSESSMENT Collecting subjective and objective data DIAGNOSIS Analyzing subjective and objective data to make a professional nursing judgment PLANNING Determining outcome criteria and developing plan IMPLEMENTATION Carrying out the plan EVALUATION Assessing whether outcome criteria have been met and revising the plan as necessary CHARACTERISTIC OF THE NURSING PROCESS Cyclic and dynamic Client centeredness Focus on problem solving and decision making. Interpersonal and collaborative style Universal applicability Use of critical thinking BENEFITS OF NURSING PROCESS Provides an orderly &systematic method for planning &providing care. Enhances nursing efficiency by standardizing nursing practice. Facilitates documentation of care. Provides a unity of language for the nursing profession. Stresses the independent function of nurses. Increases care quality through the use of deliberate actions.
o Collect data o Organize data o Validate data o Document data The first and most critical phase of the nursing process. Defined as a systematic and continuous collection, organization, validation, and documentation of data. Ongoing and continuous throughout all phases of the nursing process. FOUR TYPES OF ASSESSMENT
1. Initial Comprehensive Assessment Performed within a specified time after admission. Establish a complete database for problem identification, reference &future comparison. Involves collection of subjective data about client’s perception of his health of all body parts or systems, past health history, family history and lifestyle and health practices as well as objective data gathered during physical examination.
o Also referred to as symptoms or covert data, are apparent only to the person affected and can be described only by that person. Ex: Itching, pain and feelings of worry o Include: Client’s sensations, feelings, values, beliefs, attitudes, perception of personal health status and life situation.
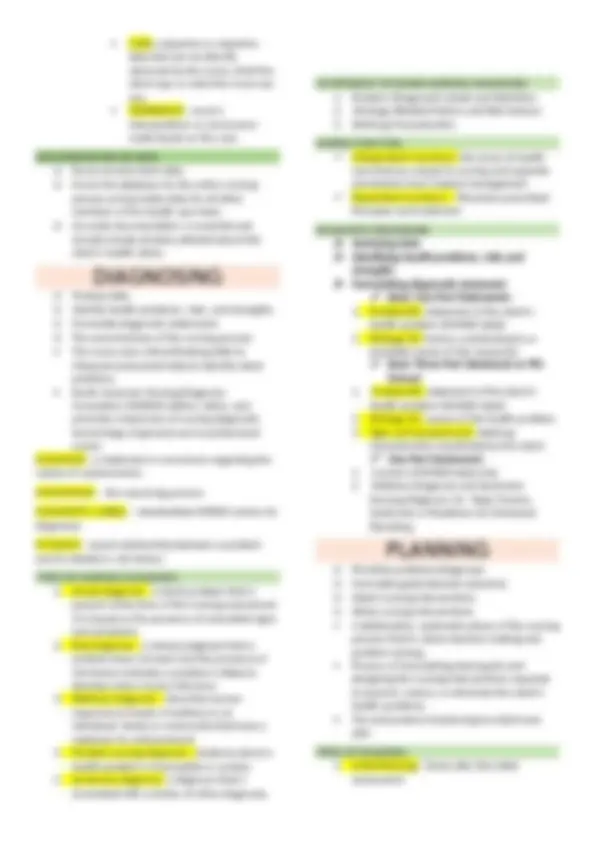
o Reassessing the client o Determining the nurse’s need for assistance. o Implementing the nursing interventions o Supervising the delegated care o Documenting nursing activities Action phase in which the nurse performs the nursing intervention. Consists of doing and documenting the activities that are the specific nursing actions needed to carry out the interventions. IMPLEMENTING SKILLS:
o Collecting data related to desired outcomes. o Comparing data with desired outcomes o Relating nursing activities to outcomes o Drawing conclusions about problem status o Continuing, modifying, or terminating the nursing care plan. Planned, ongoing, purposeful activity in which clients and healthcare professionals determine: a. The client’s progress toward achievements of goals/outcomes. b. The effectiveness of the nursing care plan. EVALUATING THE QUILITY OF NURSING CARE: Quality Assurance Ongoing, systematic process designed to evaluate and promote excellence in the health care provided to clients. Three Components of Care to be Evaluated:
**_1. Structure Evaluation