










































































Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
NURS 661 STUDY REVIEW NOTESNURS 661 STUDY REVIEW NOTES
Typology: Study Guides, Projects, Research
1 / 207

This page cannot be seen from the preview
Don't miss anything!













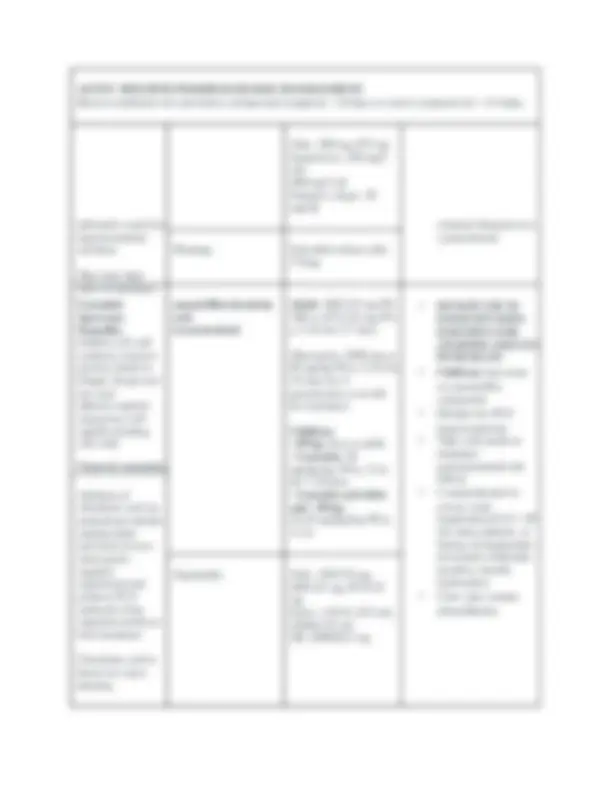













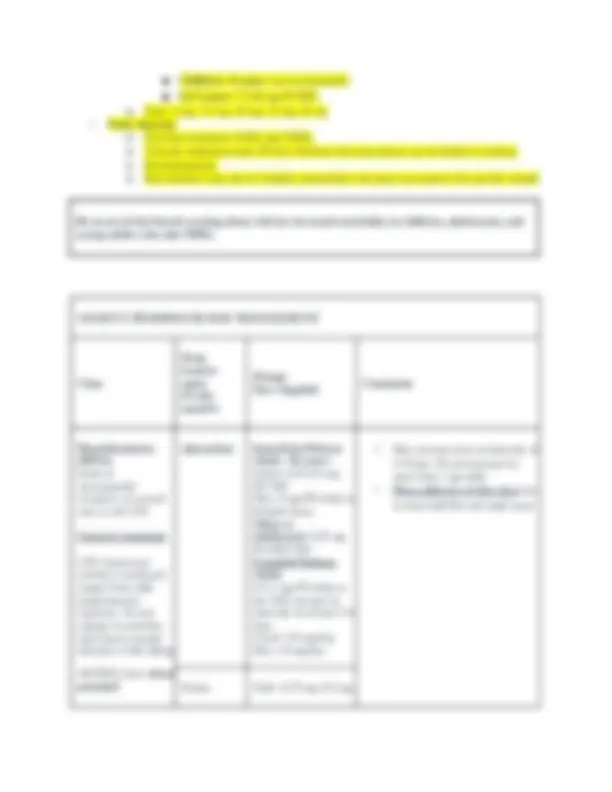















































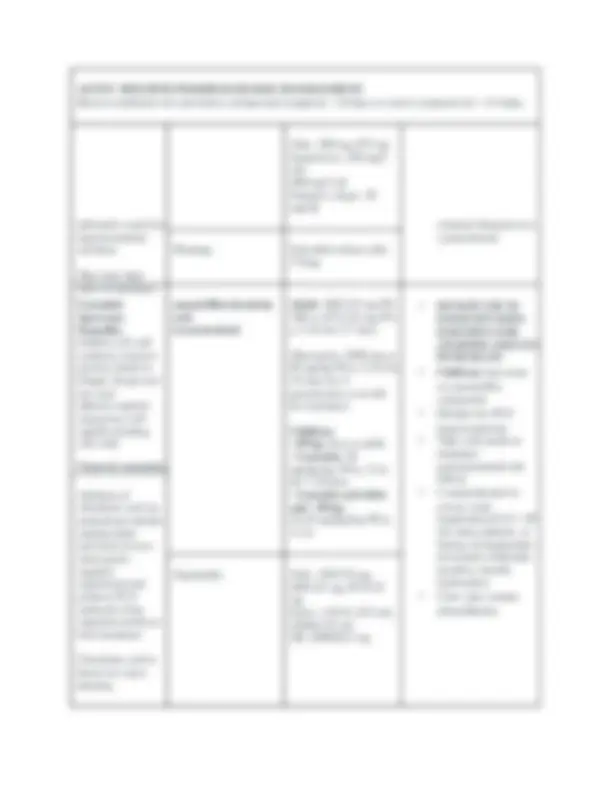
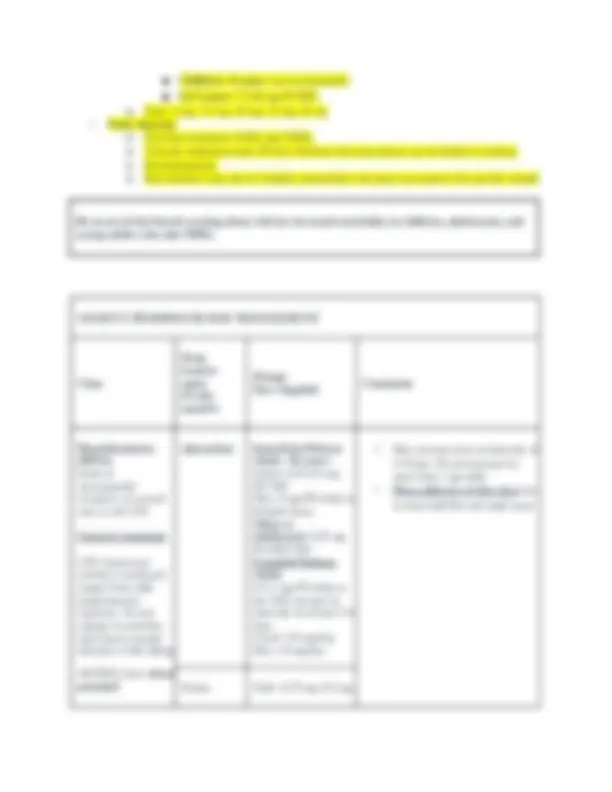
Know presentation, DX and Management
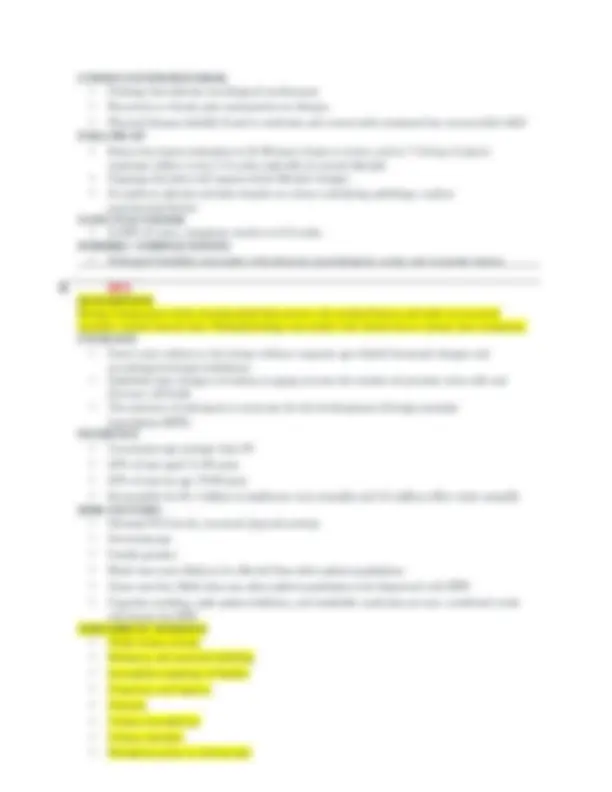
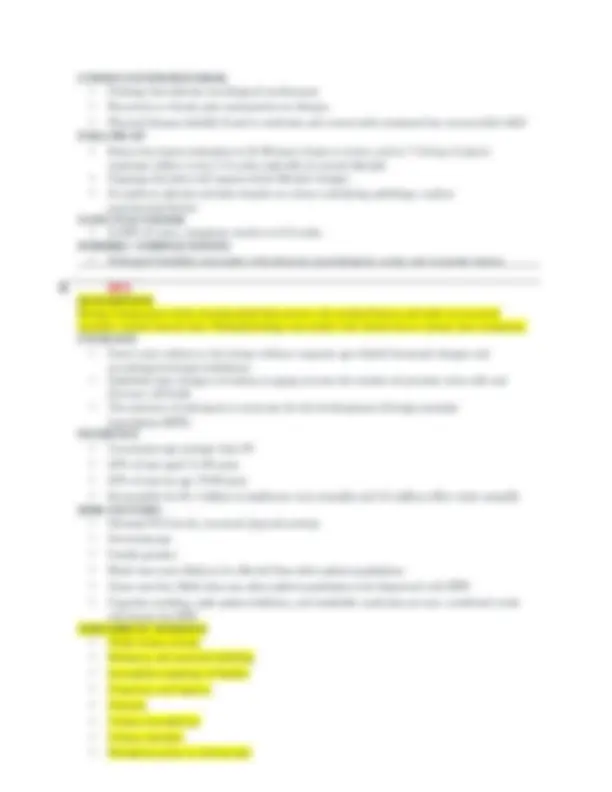
Diagnoses List
1. Acute
bronchitis-
Acute cough due to inflammation of the bronchioles, bronchi, and trachea; usually follows an upper
respiratory infection or exposure to a chemical irritant.
Although antibiotics are commonly prescribed, they are NOT recommended.
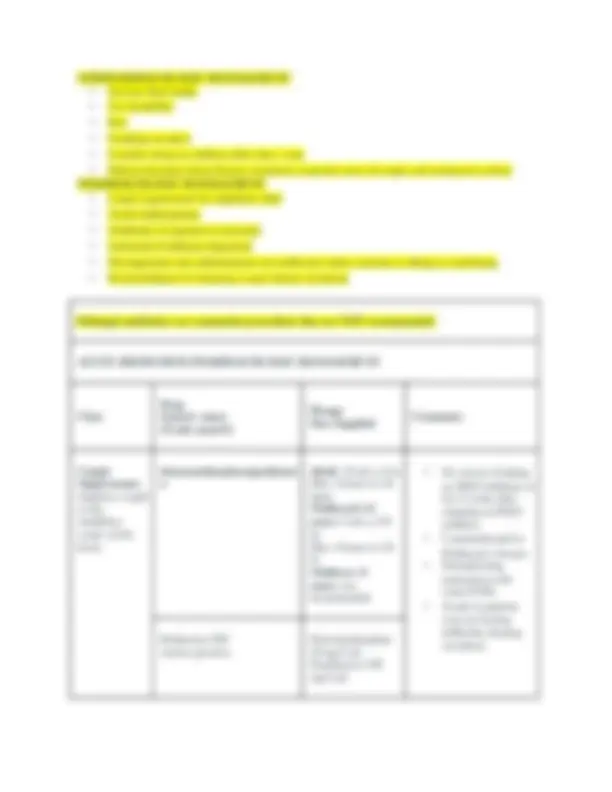
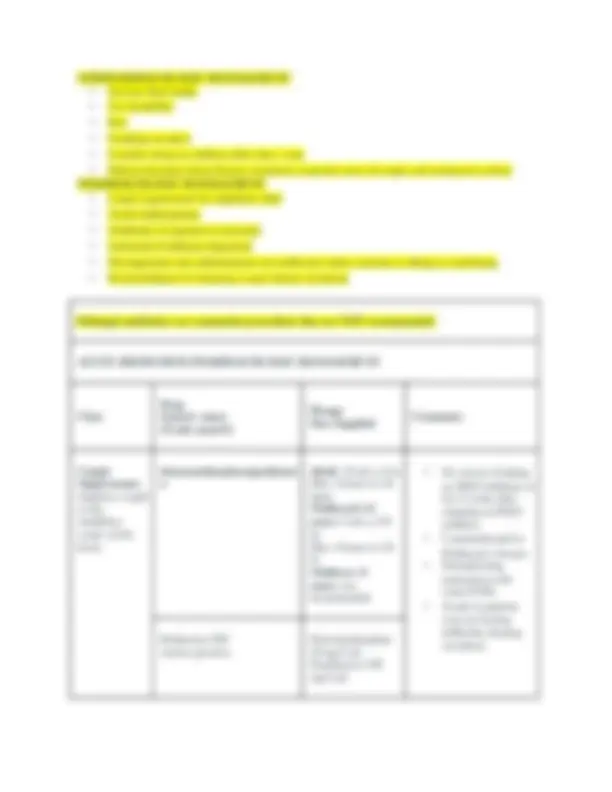
dextromethorphan Adult and ≥
years: 10 mL q 6-
hr prn for cough
Max : 4 doses in 24
hr
Children 6- 12
years: 5 mL every 6-
8 hr prn for cough
Max : 4 doses in 24
hr
4-6 years: 2.5 mL
every 6-8 hr prn for
cough
Max : 4 doses in 24
hr
an MAO inhibitor or
for 2 weeks after
stopping an MAO
inhibitor
Parkinson’s disease
intervention with
some SSRIs
who are having
difficulty clearing
secretions
sodium restricted
diet Delsym Dextromethorphan
15 mg/5 mL (alcohol
free/orange or grape
flavor)
Adult : 10 mL q 12
hr
Children 6- 12
years: 5 mL q 12 hr
Children 4- 6
years: 2.5 mL q 12
hr
codeine/guaifenesin Adults and children
≥ 12 years: 10 mL q
4 hr prn cough
Max : 6 doses in 24
hr
Children 6- 12
years: 5 mL q 4 hr
prn cough
Max : 6 doses in 24
an MAO inhibitor or
for 2 weeks after
stopping an MAO
inhibitor
Parkinson’s disease
interaction with
Although antibiotics are commonly prescribed, they are NOT recommended.
hr some SSRIs
medication
who are having
difficulty clearing
secretions
suppressants in
patient with COPD or
asthma
forming
constipation
Robitussin AC Each 5 mL contains
100 mg guaifenesin
and
10 mg codeine
Antitussives
Topical
anesthetic effect
on the
respiratory
stretch
receptors
benzonatate Adults and children
> 10 years:
100-200 mg TID prn
cough
Max: 600 mg daily
chew capsule - can
produce local
anesthesia and may
reduce patient’s gag
reflex
dizziness,
drowsiness and
visual changes
20 minutes and lasts
for 3-8 hours
sensitive to or taking
agents with PABA -
possible adverse
CNS effects
Tessalon Caps: 100 mg, 200
mg
Expectorants guaifenesin Adult : 200-400 mg
PO q 4 hr prn
Max: 2400 mg/day
Children 2- 5
nephrolithiasis
Although antibiotics are commonly prescribed, they are NOT recommended.
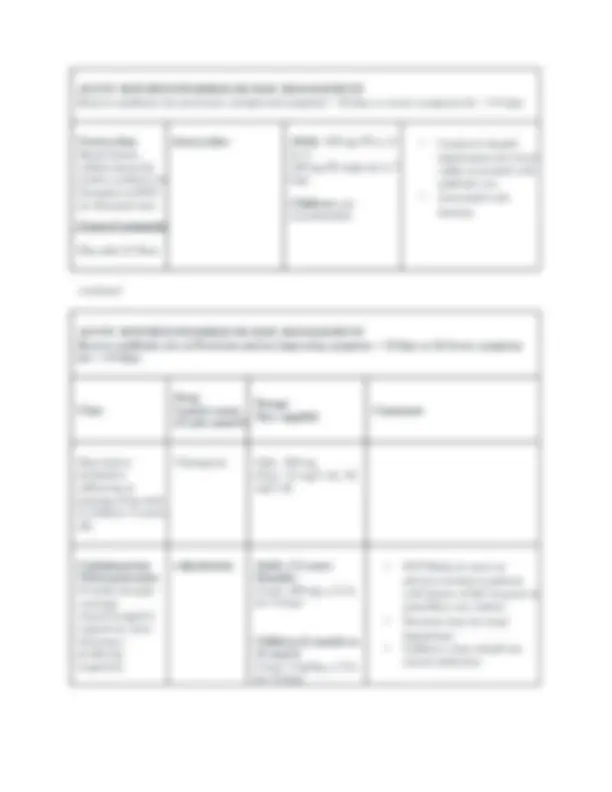
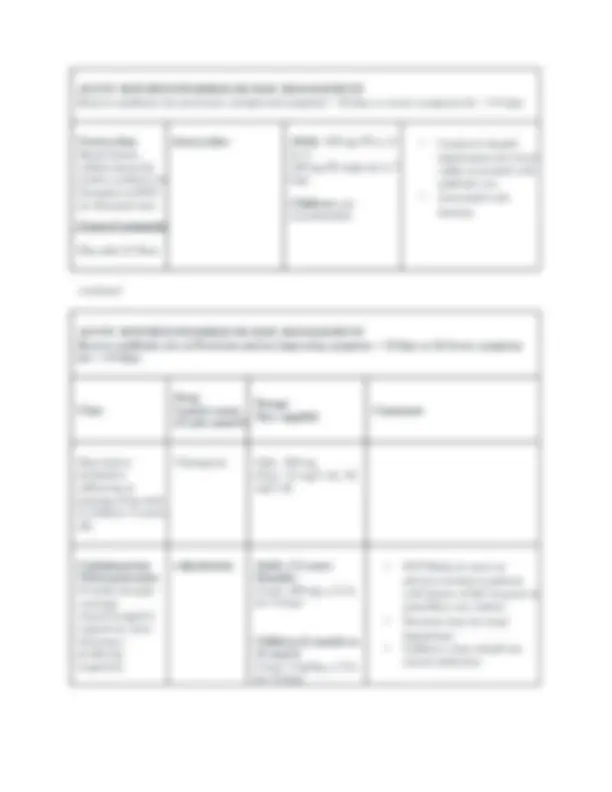
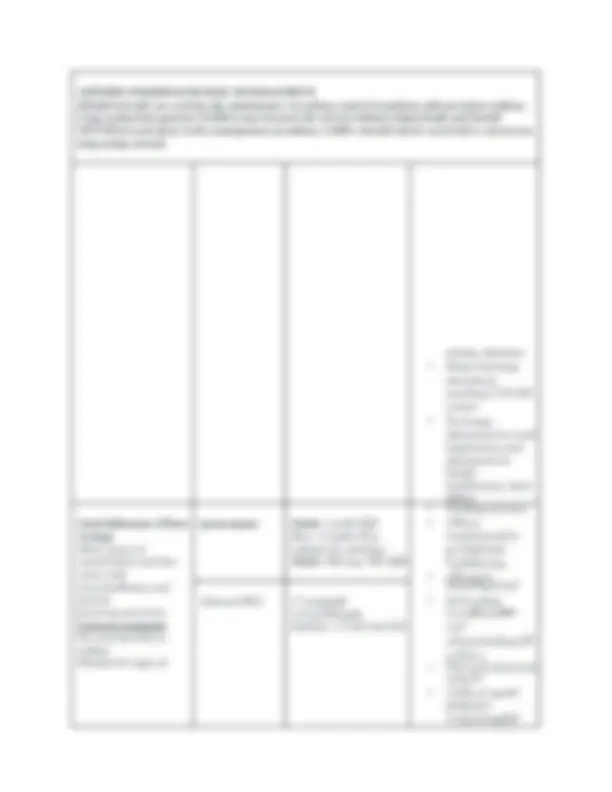
Max: 8 inhalations
daily
Dry powder inhaler
mcg/inhalation):
Acute treatment: 1
inhalation (200 mcg)
as needed; Max: 4
inhalations (
mcg)/day; patient
should be advised to
promptly consult
health care provider
or seek medical
attention if prior
dose fails to provide
adequate relief or if
control of symptoms
lasts <3 hr
Maintenance (in
combination with
corticosteroid
therapy): 1
inhalation (200 mcg)
q 4-6 hr; Max : 4
inhalations (
mcg)/day
Nebulization
solution: 2.5 mg
TID-QID as needed;
Quick relief: 1.25 to
5 mg q 4-8 hr as
needed (NAEPP
Pediatric:
Inhalation:
Metered-dose
inhaler or dry
powder inhaler (
mcg/actuation) quic
k relief: refer to
adult dosing for all
dry
completely
prior to use.
A spacer
device or
valved
holding
chamber is
recommende
d for use
with
metered-
dose
inhalers.
o Metered-
dose inhalers
aerosols):
Store at
15°C to
to 77°F). Do
not store at
temperature
120°F. Do
not puncture.
Do not use
or store near
heat or open
flame.
Discard when
counter reads 000 or
12 months after
removal from
protective pouch,
whichever comes
first. Store with
mouthpiece down.
patients with
Although antibiotics are commonly prescribed, they are NOT recommended.
ages
Metered-dose
inhaler (
mcg/actuation):
Children 6 to 11
years:
Acute treatment: 1
inhalation; additional
inhalations may be
necessary if
inadequate relief;
however, patients
should be advised to
promptly consult
health care provider
or seek medical
attention if no relief
from acute treatment
Maintenance (in
combination with
corticosteroid
therapy): 1
inhalation; may
increase to
maximum of 1
inhalation QID
Children ≥12 years
and
adolescents: refer to
adult dosing
impaired renal
disease,
hyperthyroidism,
diabetes, glaucoma
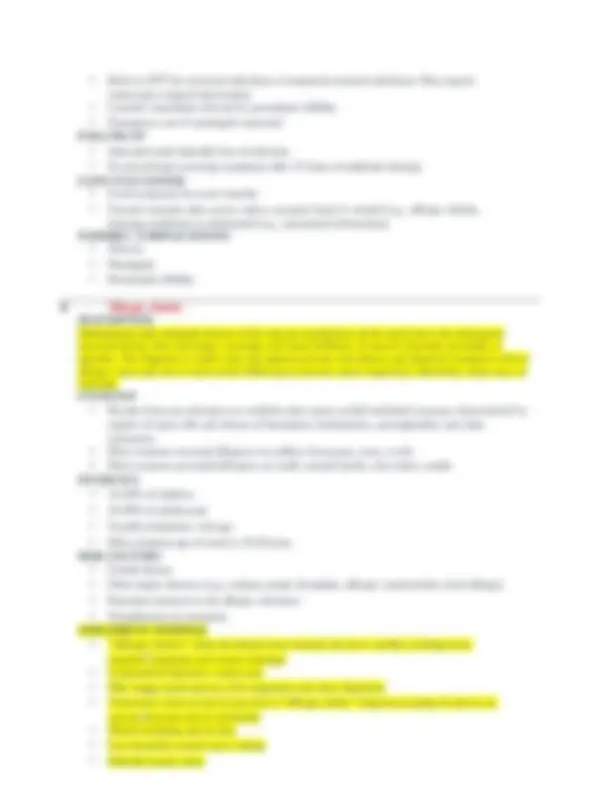
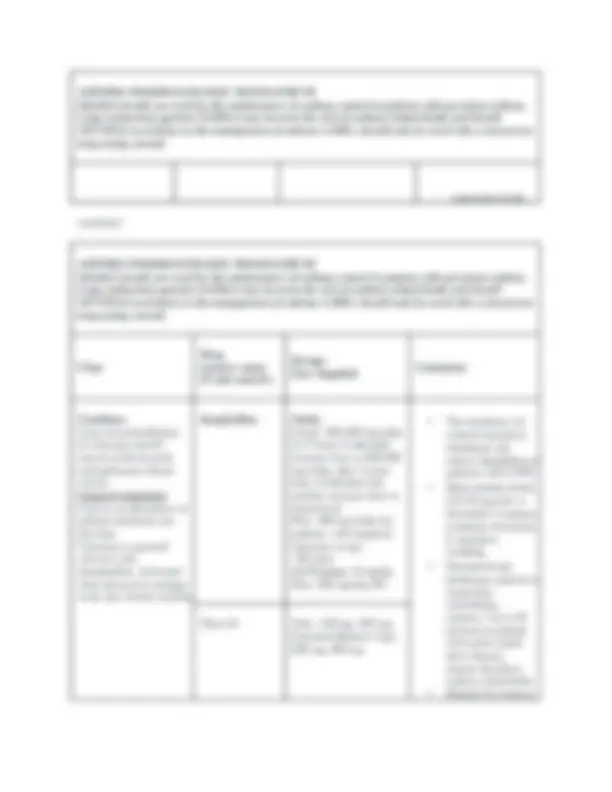
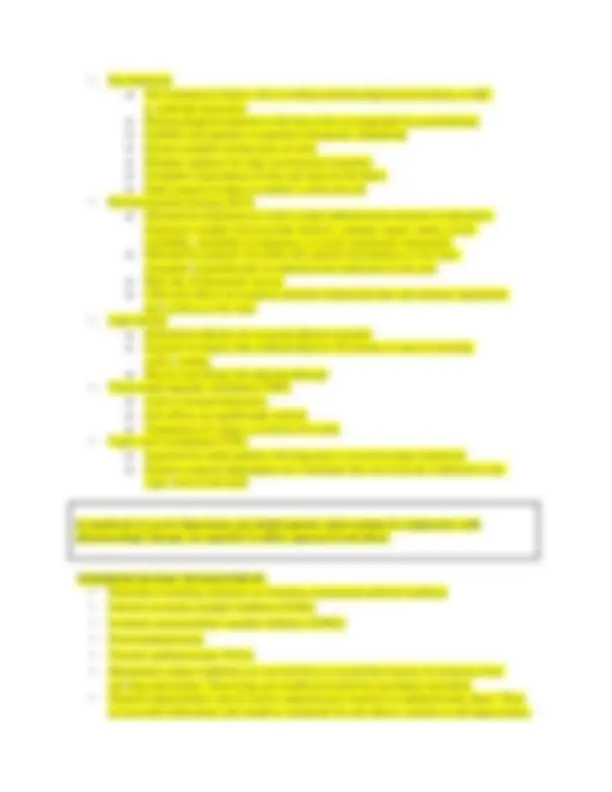
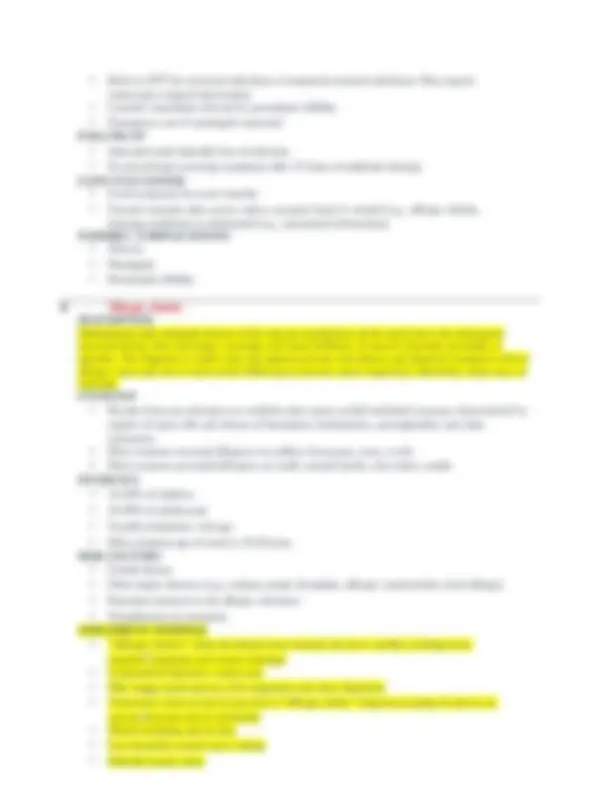
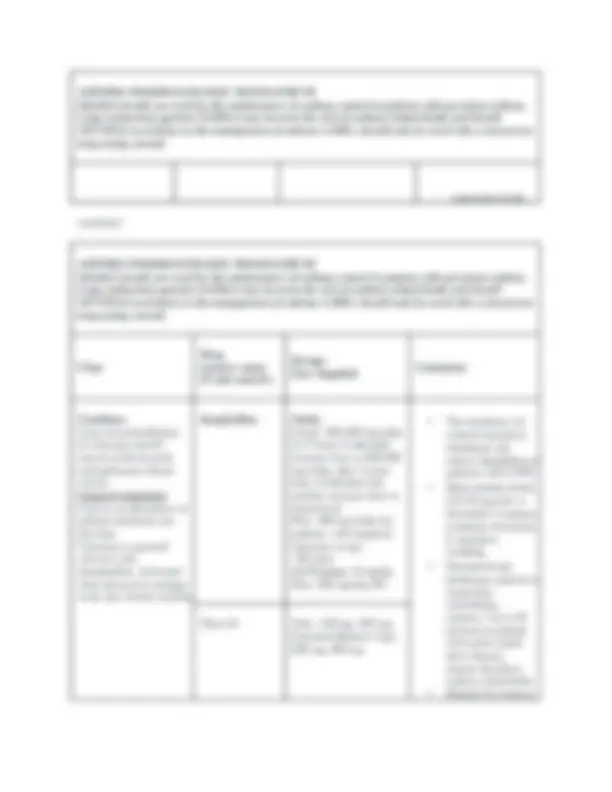
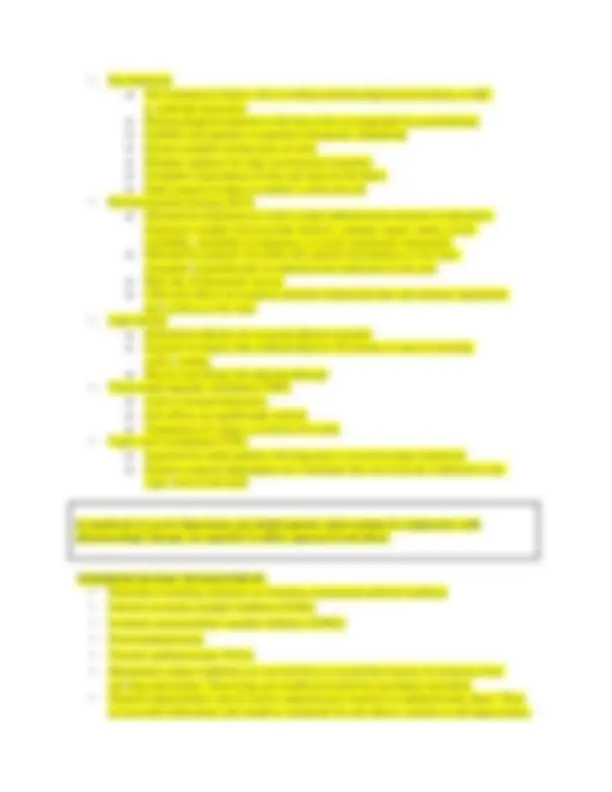
An acute inflammation of the pharynx/tonsils. The most common cause of acute pharyngitis is viruses.
Accurate diagnosis and treatment of Strep pharyngitis is important to prevent rheumatic fever,
poststreptococcal glomerulonephritis, to reduce transmission, and to limit complications, such as
peritonsillar abscess, lymphadenitis, and mastoiditis
Causes
Viral Bacterial*
* Most common etiology
** Common depending on time of year
symptoms of strep pharyngitis and other etiologies overlap, and an accurate diagnosis based
on clinical findings alone is difficult
o Cervical adenopathy
o Fever >102° F (38.8° C)
o Absence of other upper respiratory findings (cough, nasal congestion, etc.)
o Petechiae on soft palate
o “Beefy red” tonsils
o “Sandpaper” rash (bridge of nose, neck, and/or torso)
o Abdominal pain, headache
o Streptococcal tonsillitis has a distinct odor
o Concurrent conjunctivitis, nasal congestion, hoarseness, cough, diarrhea or viral rash
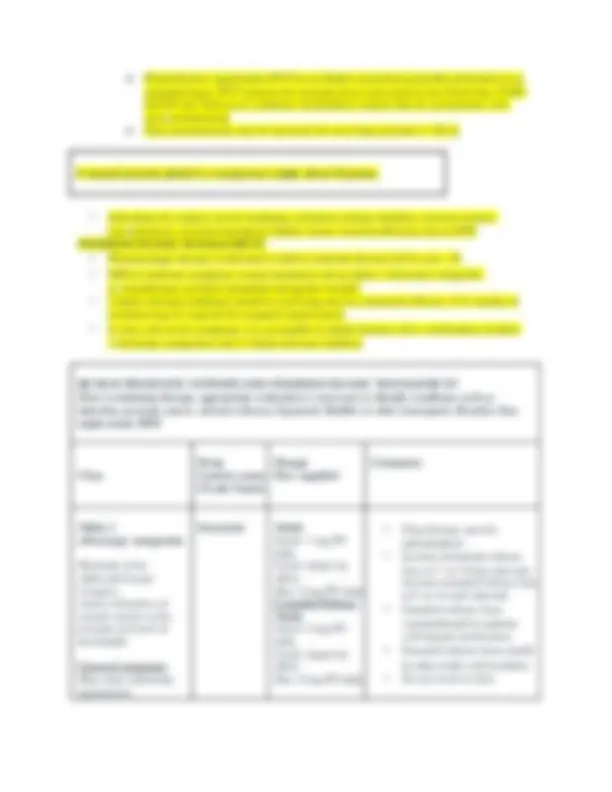
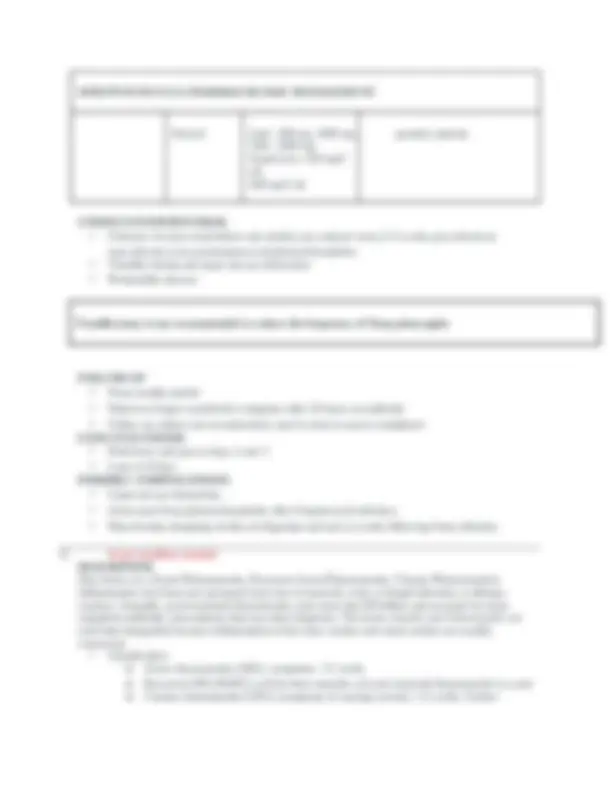
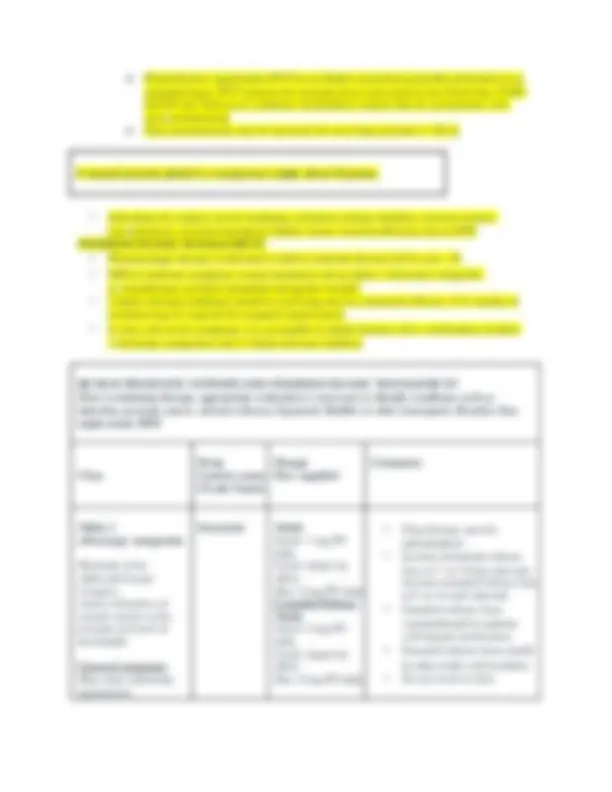
Modified Centor Clinical Prediction Rule for Group A Strep infection
Tonsillar exudates +1 point
Tender anterior chain cervical adenopathy +1 point
Fever by history +1 point
Age <15 years +1 point
Age 15- 45 0 points
Age >45 -1 point
Cough (almost always excludes Streptococcus ) -1 point
3-4 points: treat empirically for Strep infection
2 points: rapid Strep test, treat if positive
1 point: unlikely Strep
0 or -1 points: do not test or treat
wall. Good specimen is essential
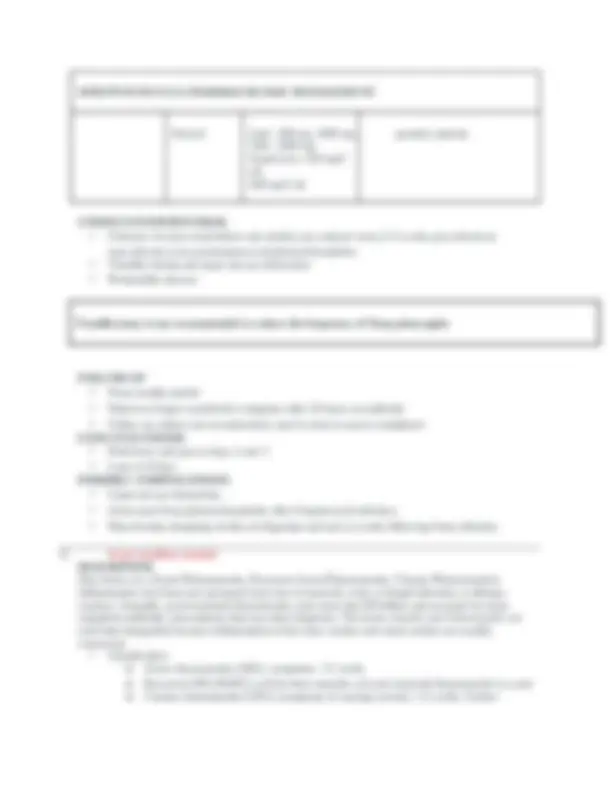
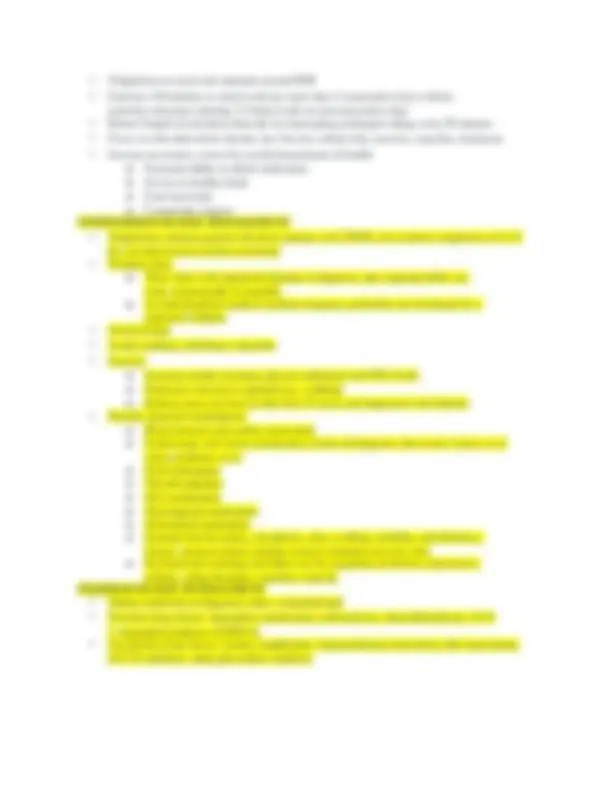
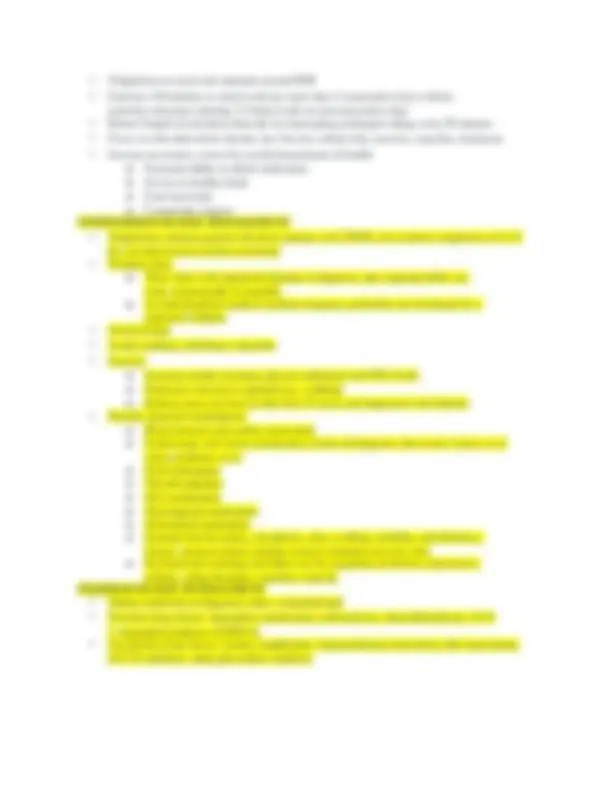
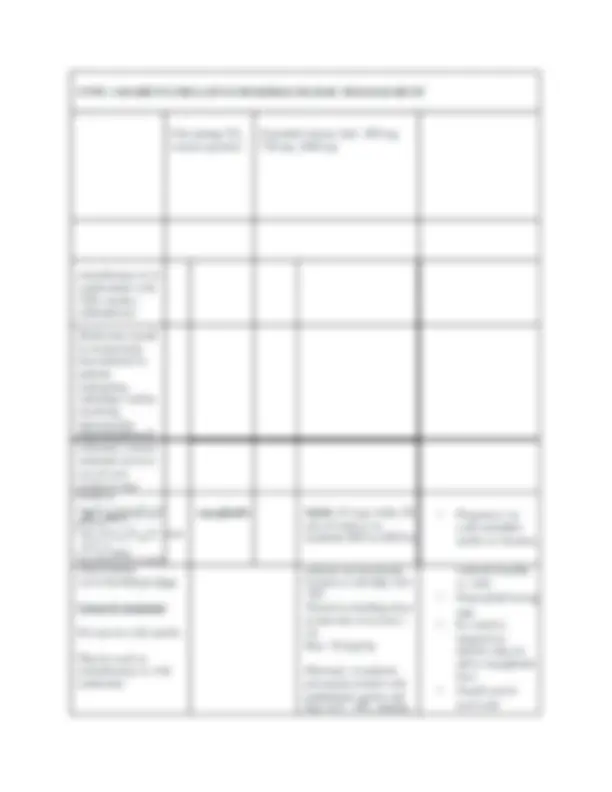
Penicillin G One IM injection
Medication (based on patient’s age or weight) Treatment
Penicillin V
Amoxicillin
Requires 10 days of treatment
First-generation
cephalosporins
Requires 10 days of treatment
Second-generation
cephalosporins
5 days of treatment
Azithromycin (for PCN allergy); limited efficacy
against Streptococcal infection and should only be
used for patients with documented history of PCN
anaphylaxis or hives
12 mg/kg dose daily x 5 days
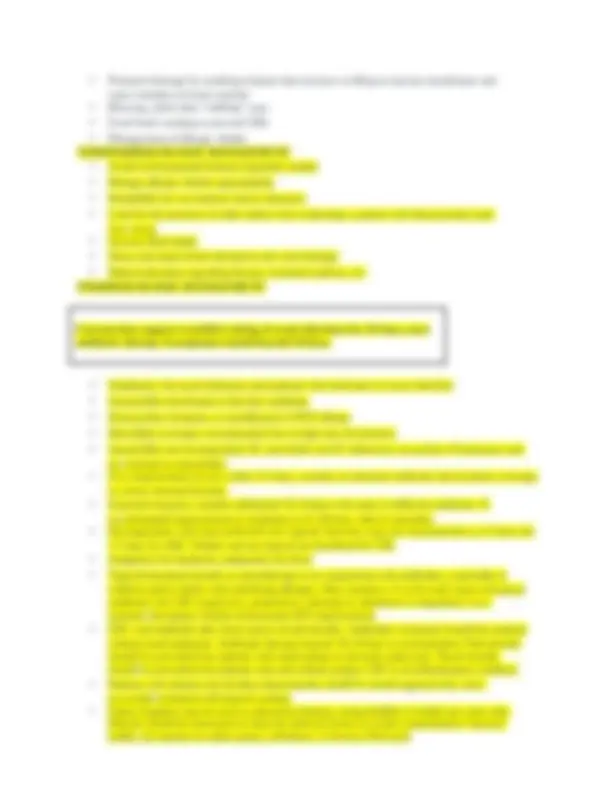
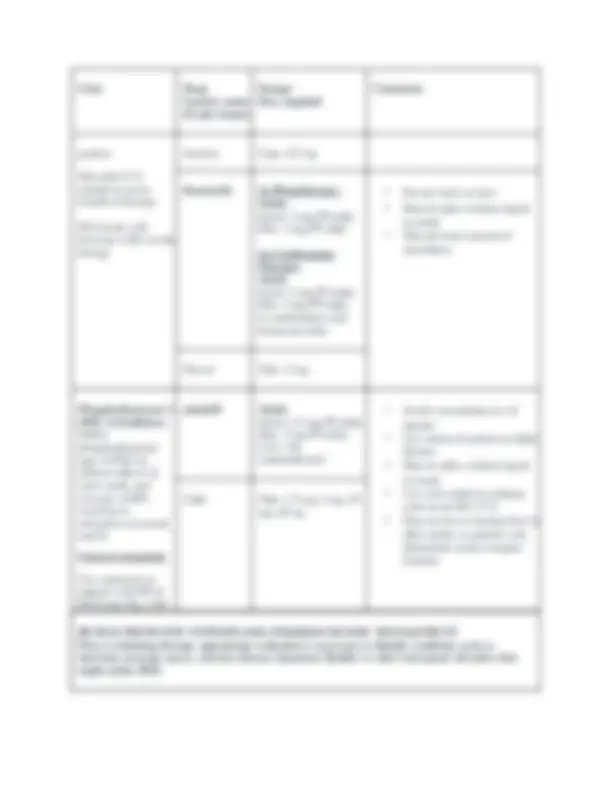
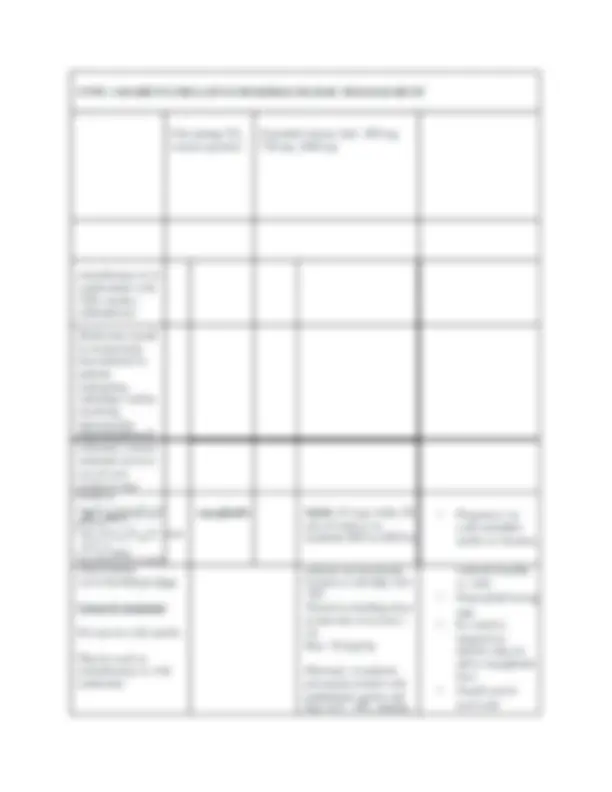
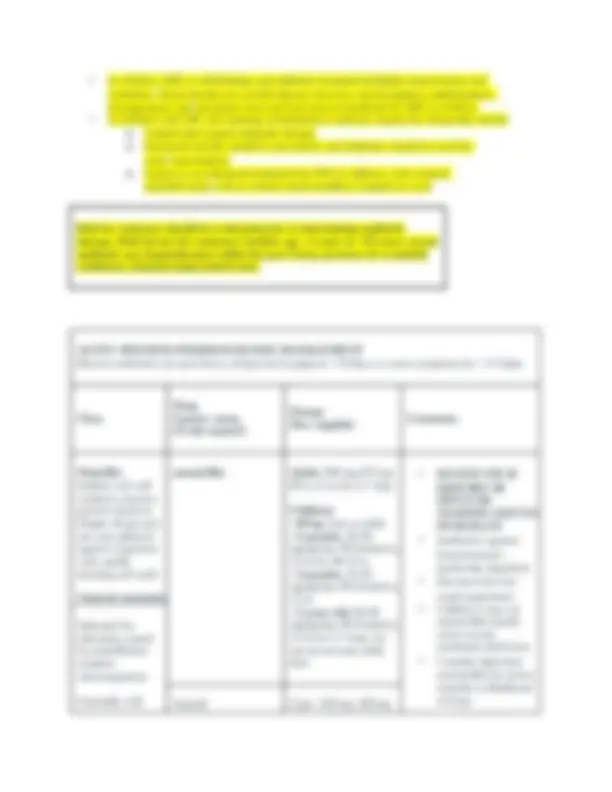
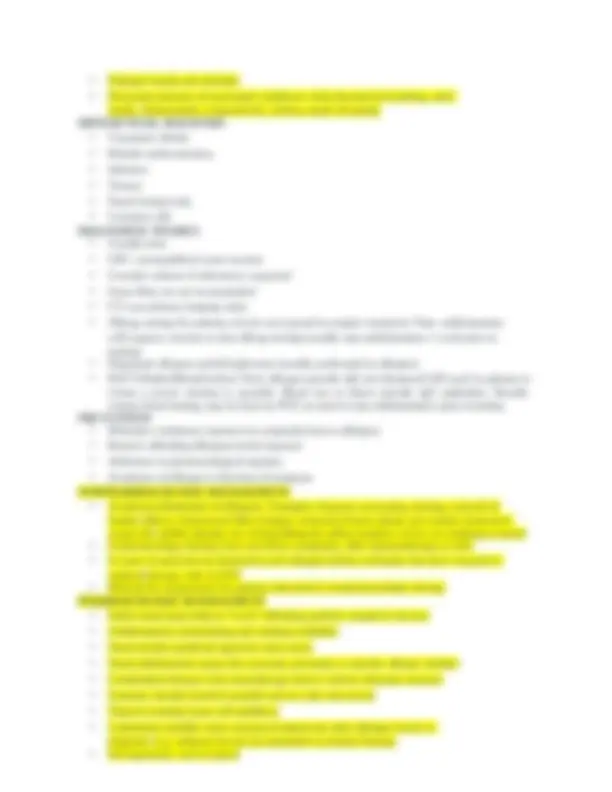
Class
Drug
Generic
name
(Trade
name®)
Dosage
How supplied
Comments
Penicillin Bacterial;
Bactericidal: inhibits
cell wall mucopeptide
synthesis; inhibits
beta-lactamase
General comments
penicillin V
potassium
Adult: 500 mg 2-
times daily for 10 days
Children: 250 mg PO
BID-TID for 10 days
Adolescents: 500 mg
PO BID for 10 days
after meals
Indicated for infections
caused by
penicillinase-sensitive
Pen V K Tablet: 250 mg, 500
mg
Oral Solution: 125
mg/5 mL, 250 mg/5 mL
penicillin G
benzathine
Adult: 1.2 million
units IM for 1 dose
<27 kg: 0.6 million
units IM for 1 dose
≥27 kg: 1.2 million
units IM for 1 dose
with Bicillin C-R
benzathine with penicillamine
or penicillin G procaine. They
are NOT interchangeable
combined with Penicillin G
procaine (Ex. 900,000 units of
Penicillin G benzathine +
300,000 units of Penicillin G
procaine = 1.2 million units)
Bicillin L-A Injection: 600,
units/mL, 1.2 million
units/2 mL
microorganisms
amoxicillin Adult: 500-875 mg PO
q 12 hr for 10-
days (higher dosing for
severe infections)
presence of beta lactamase
producing organisms
impairment
should never exceed maximum
adult dose
Generally well
tolerated; watch for
hypersensitivity
reactions
Clavulanate broadens
spectrum of coverage
Consider
amoxicillin/clavulanate
if failure after 72 hours
Children:
>40 kg: dose for 10
days
50 mg/kg once daily
for 10 days
Max: 1 g/day
Alternate: 25 mg/kg
BID for 10 days
Max: 500 mg/dose
The course of treatment
is 10 days for all beta-
lactam antibiotics, but
Moxatag 775 mg ER Tab daily
for 10 days
continued
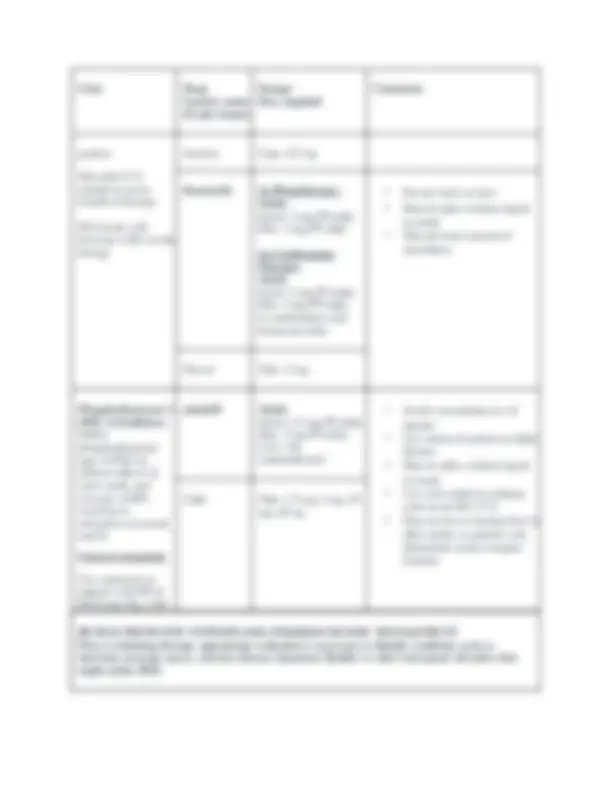
Class
Drug
Generic name
(Trade name®)
Dosage
How supplied
Comments
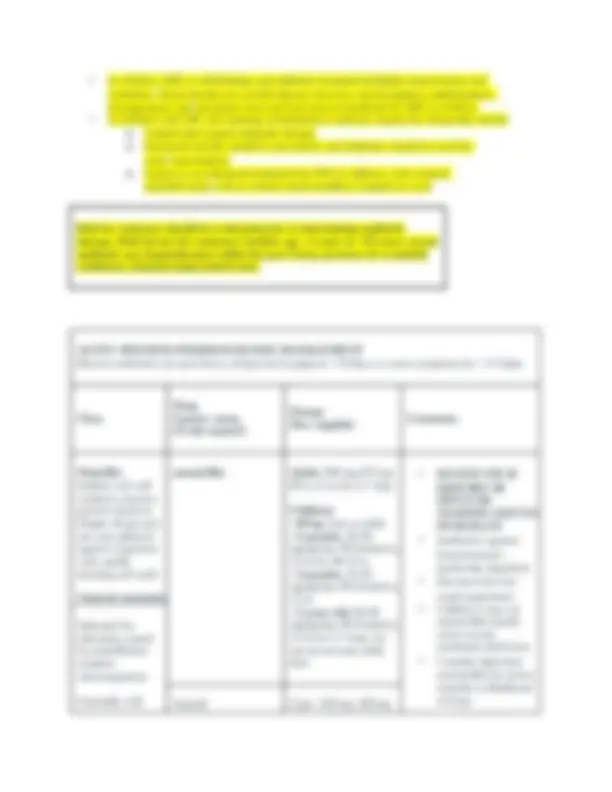
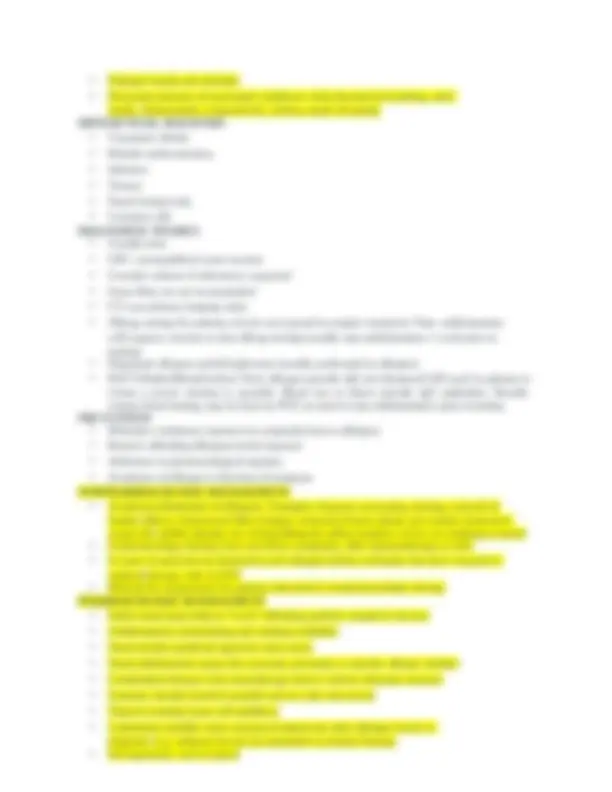
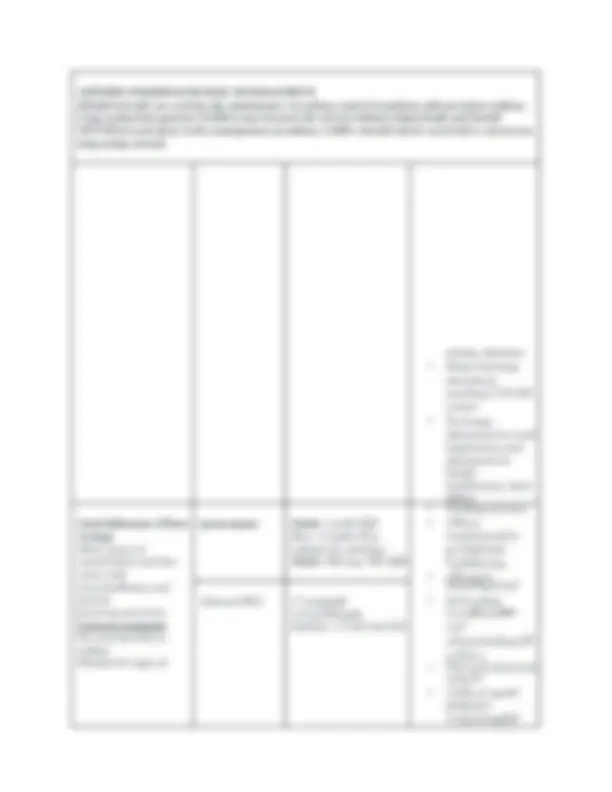
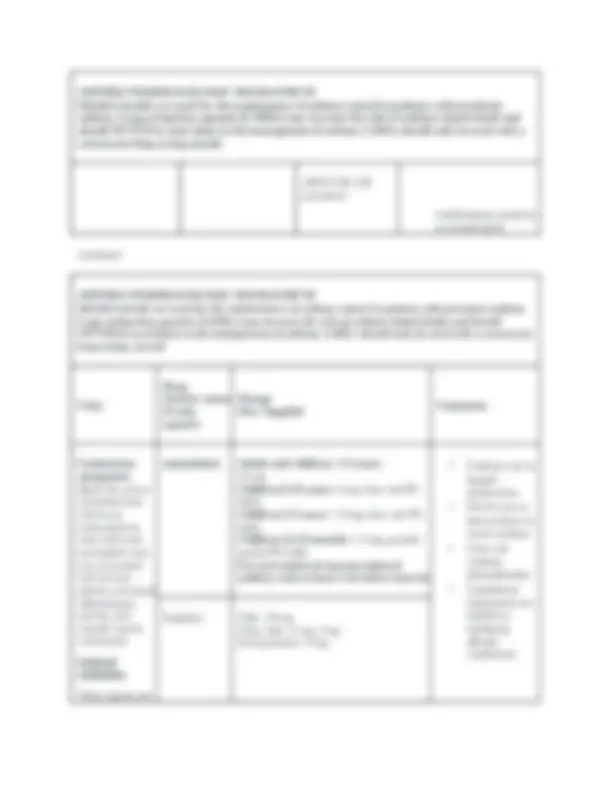
Macrolides
Inhibits bacterial
growth, possibly
by blocking
dissociation of
peptidyl tRNA
from ribosomes,
causing RNA-
dependent protein
synthesis to arrest
General
comments
Effective treatment
for S. pyogenes in
the presence of
penicillin allergy
Associated with
higher rates of GI
side effects
azithromycin Adult:
Usual : 500 mg daily
for 3 days
Alternative: 2 g as a
single dose or 500 mg
on day 1 and 250 mg
days 2- 5
Children >6 months
old:
Usual: 10 mg/kg once
daily for 3 days or 10
mg/kg on day 1 and 5
mg/kg days 2- 5
Max: 500 mg daily
(Type I allergic reaction)
after 48-72 hours
aluminum or magnesium
containing antacids
impairment
recur after initial successful
symptomatic treatment
Zithromax Tabs: 500 mg, 250 mg
Powder: 2 g/bottle
Suspension: 100 mg/
mL,
200 mg/5 mL
Age, weight and
severity of
infection
determine dose in
children
Local antibiotic
resistant rates
should be
clarithromycin Adult: 250 mg PO q
12 hr for 10 days
Children 6 months
and older:
15 mg/kg/day PO
divided q 12 hr for 10
days
Max: 250 mg/dose
either renal or hepatic
dysfunction
in drug reactions involving CYP
450 system; special care when
prescribing concurrently with
3A4 substrate medications
abnormal taste in mouth while
taking tablet or suspension
Biaxin Coated tabs: 250 mg,
500 mg
Biaxin XL Coated tabs extended
release: 500 mg
Other
Antibacterials
Bacteriostatic or
bactericidal,
inhibits protein
synthesis
General
comments
Half-life is 2.4-
hours
Carries a black
box warning
for C.
difficile associated
diarrhea
clindamycin Adult: 300 mg PO q 8
hr for 10 days
Children: 7
mg/kg/day PO divided
q 8 hr for 10 days
Max: 300 mg/dose
Adolescents: 150-
mg PO q 6 hr
Max 300 mg per dose
been unsuccessful
bacterial failure who are
penicillin/cephalosporin allergic
with Type I reaction; consider
use in patients who failed therapy
with ceftriaxone (used in
conjunction with
tympanocentesis)
continued
Duricef Caps: 500 mg, 1000 mg,
Tabs: 1000 mg
Suspension: 250 mg/
mL,
500 mg/5 mL
geriatric patients
may indicate acute poststreptococcal glomerulonephritis
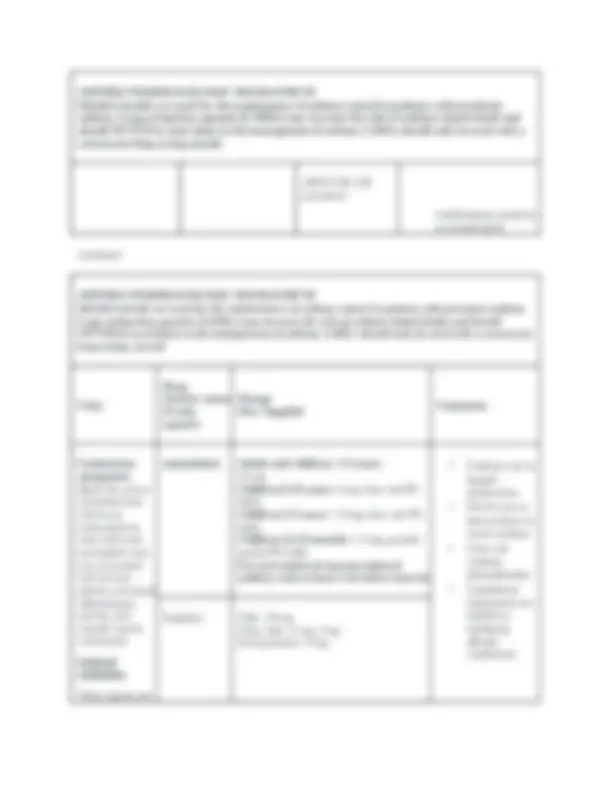
Also known as: (Acute Rhinosinusitis, Recurrent Acute Rhinosinusitis, Chronic Rhinosinusitis)
Inflammation of at least one paranasal sinus due to bacterial, viral, or fungal infection; or allergic
reaction. Annually, acute bacterial rhinosinusitis costs more than $3 billion and accounts for more
outpatient antibiotic prescriptions than any other diagnosis. The terms sinusitis and rhinosinusitis are
used interchangeably because inflammation of the sinus cavities and nasal cavities are usually
concurrent.
o Acute rhinosinusitis (ARS): symptoms <12 weeks
o Recurrent ARS (RARS): at least three episodes of acute bacterial rhinosinusitis in a year
o Chronic rhinosinusitis (CRS): symptoms of varying severity >12 weeks. Further
Tonsillectomy is not recommended to reduce the frequency of Strep pharyngitis
classified with or without nasal polyps; abnormal findings on CT scan or nasal
endoscopy